
You will perform a history of an abdominal problem that your instructor has provided you
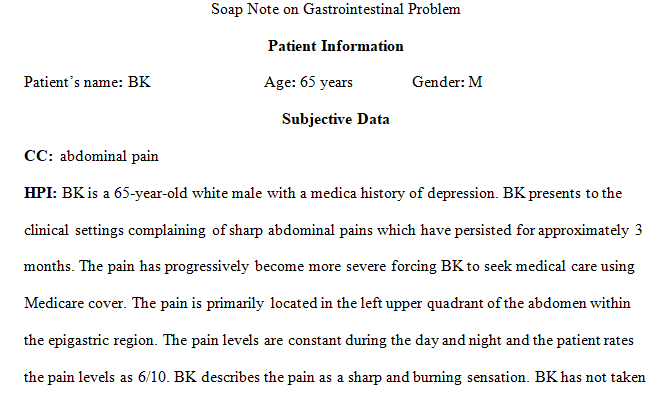
Soap Note on Gastrointestinal Problem
You will perform a history of an abdominal problem that your instructor has provided you or one that you have experienced and perform an assessment including nose, mouth, throat, and neck. You will document your subjective and objective findings, note any abnormal findings, and submit this in a Word document to the drop box provided.
Remember to be objective when you document; do not make judgments. For example, if the person has a palpably enlarged liver, do not write “the liver is enlarged probably because they drink too much.” Avoid stating that something is normal but instead state WHY you think it is normal. For example, if you think that the abdomen looks “normal” – which is subjective – then document that the “abdomen is flat, skin color consistent with rest of body, no lesions, scars, bulges, or pulsations noted.”
Gastrointestinal System Assignment -full instructions attached
Submit your completed assignment by following the directions linked below. Please check the Course Calendar for specific due dates.
Title:
Documentation of problem based assessment of the gastrointestinal system.
Purpose of Assignment:
Learning the required components of documenting a problem based subjective and objective assessment of gastrointestinal system. Identify abnormal findings.
Course Competency:
Prioritize appropriate assessment techniques for the gastrointestinal, breasts, and genitourinary systems.
Instructions:
Content:
- Use of three sections: Subjective, Objective, and Abnormal Findings
- Short descriptive paragraph of findings for each section
Format:
- Standard American English (correct grammar, punctuation, etc.)
Resources:
Chapter 5: SOAP Notes: The subjective and objective portion only
Sullivan, D. D. (2012). Guide to clinical documentation. [E-Book]. Retrieved from http://ezproxy.rasmussen.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=nlebk&AN=495456&site=eds-live&ebv=EB&ppid=pp_91 >
Smith, L. S. (2001, September). Documentation do’s and don’ts. Nursing, 31(9), 30. Retrieved from http://ezproxy.rasmussen.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=107055742&site=eds-live
Documentation Grading Rubric- 10 possible points
| Levels of Achievement | ||||
| Criteria | Emerging | Competence | Proficiency | Mastery |
| Subjective
(4 Pts) |
Missing components such as biographic data, medications, or allergies. Symptoms analysis is incomplete. May contain objective data. | Basic biographic data provided. Medications and allergies included. Symptoms analysis incomplete. Lacking detail. No objective data. | Basic biographic data provided. Included list of medications and allergies. Symptoms analysis: PQRSTU completed. Lacking detail. No objective data. Information is solely what “client” provided. | Basic biographic data provided. Included list of medications and allergies. Symptoms analysis: PQRSTU completed. Detailed. No objective data. Information is solely what “client” provided. |
| Points: 0.5 | Points:1 | Points: 2 | Points: 4 | |
| Objective
(4 Pts) |
Missing components of assessment for particular system. May contain subjective data. May have signs of bias or explanation of findings. May have included words such as “normal”, “appropriate”, “okay”, and “good”. |
Includes all components of assessment for particular system. Lacks detail. Uses words such as “normal”, “appropriate”, or “good”.Contains all objective information. May have signs of bias or explanation of findings. | Includes all components of assessment for particular system. Avoided use of words such as “normal”, “appropriate”, or “good”.No bias or explanation for findings evident Contains all objective information | Includes all components of assessment for particular system. Detailed information provided.Avoided use of words such as “normal”, “appropriate”, or “good”.No bias or explanation for findings evident. All objective information |
| Points: 1 | Points: 2 | Points: 3 | Points: 4 | |
| Strength and Weakness
(2 Pts) |
Lists one strength and one weakness with no description or reason for selection of them. Failure to provide both one strength and weakness will result in zero points for this criteria. | Provides brief description of one strength and one weakness with no reason for identification of the strength and weakness. | Provides description of one strength and one weakness noted on assessment. Gives reason for identification of the strength and weakness. | Detailed description of one strength and one weakness noted during assessment. Detailed reason provided for identifying the strength and weakness. |
| Points: 0.5 | Points: 1 | Points: 1.5 | Points: 2 | |
5 hours ago
REQUIREMENTS
Rasmussen NUR2180 Section Q2 Physical Assessment
Nursing
Answer preview……………………..
apa 849 words