
You will perform a history of an abdominal problem that your instructor has provided you or one that you have experienced and perform an assessment including nose, mouth, throat, and neck.
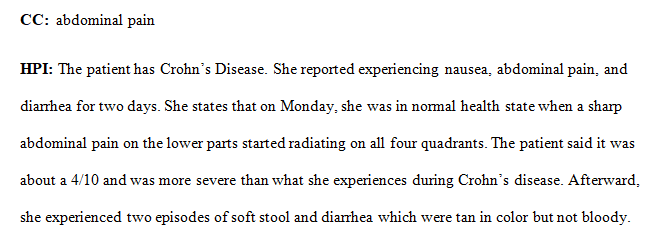
Soap Note on Gastrointestinal Problem
You will perform a history of an abdominal problem that your instructor has provided you or one that you have experienced and perform an assessment including nose, mouth, throat, and neck. You will document your subjective and objective findings, note any abnormal findings, and submit this in a Word document to the drop box provided.
Remember to be objective when you document; do not make judgments. For example, if the person has a palpably enlarged liver, do not write “the liver is enlarged probably because they drink too much.” Avoid stating that something is normal but instead state WHY you think it is normal. For example, if you think that the abdomen looks “normal” – which is subjective – then document that the “abdomen is flat, skin color consistent with rest of body, no lesions, scars, bulges, or pulsations noted.”
Gastrointestinal System Assignment -file attached
Submit your completed assignment by following the directions linked below. Please check the Course Calendar for specific due dates.
REQUIREMENTS
Rasmussen NUR2180 Section Q2 Physical Assessment
ursing
FOLLOWING THE INSTRUCTION AND RUBRIC ON THE attached document
Answer preview…………………
apa 920 words